Release date: 2014-09-04
Clinically, fetal tracheal and bronchial lesions are rare, but most of the disease is dangerous after the onset, and the fetal survival rate is very low. At present, the routine preoperative routine ultrasound examination specification has not involved trachea and bronchus, and there is less understanding of the ultrasound morphology of this area of ​​normal fetus. Occasionally, lesions are mostly dependent on indirect ultrasound signs, so the detection rate of lesions is low, and the detection time is late. A certain rate of missed diagnosis.
Recently, an article published in the Chinese Journal of Ultrasound Imaging has reviewed the anatomical features, congenital lesions and ultrasound research progress of fetal trachea and bronchi.
I. Embryonic development of the trachea and bronchi
At the 4th week of the embryo, a longitudinal groove appeared in the middle of the original pharyngeal wall, called the laryngotracheal groove. The laryngotracheal groove gradually deepens and heals from the tail end to the head end, forming a long-shaped blind sac, called the laryngotracheal diverticulum, which is located on the ventral side of the esophagus. The mesenchyme between the two is called the tracheal esophageal septum; the upper end is developed as The larynx, the middle part develops into the trachea, and the two branches that are swollen at the end are called lung buds, which are the primordium of the main bronchus and lung.
The lung buds were dendritic and repeatedly branched. At the 6th month, they reached the 17th grade, forming the lobes of the lungs, the bronchi of the lungs, the respiratory bronchioles, the alveolar duct and the alveolar sac.
Second, the anatomical basis of the trachea and bronchi
The trachea is located in the anterior middle of the neck, starting at the level of the cartilage, ending at the level of the sternum and bifurcation into two major bronchus. The right main bronchus is thicker and shorter, and the shape is steeper and straighter; the left main air tube is slender and straighter. The full-term neonatal trachea is about 4 cm long and about 3-4 mm in diameter. The side wall and front wall of the trachea are supported by 16-20 horseshoe-shaped cartilage. Tracheal cartilage is a type C hyaline cartilage.
The posterior and membranous portions of the trachea are composed of tracheal muscles, elastic tissue, and fibrous tissue. The structure of the main bronchial wall is similar to that of the trachea. The upper and lower thyroid arteries, the thymus artery, and the right bronchial artery provide arterial blood supply to the trachea. The venous venous ring travels along the cartilage space and flows back into the esophageal and subthyroid veins.
Third, ultrasound observation of normal fetal trachea and bronchus
After the baby is born, it is very difficult to display the trachea by ultrasound because of bone and gas blockage. In the fetal period, the trachea is filled with fluid produced by the lungs, and enters the amniotic fluid through the trachea and throat through respiratory movement. Therefore, ultrasound after mid-pregnancy can show that the fetal trachea has an elliptical tubular anechoic.
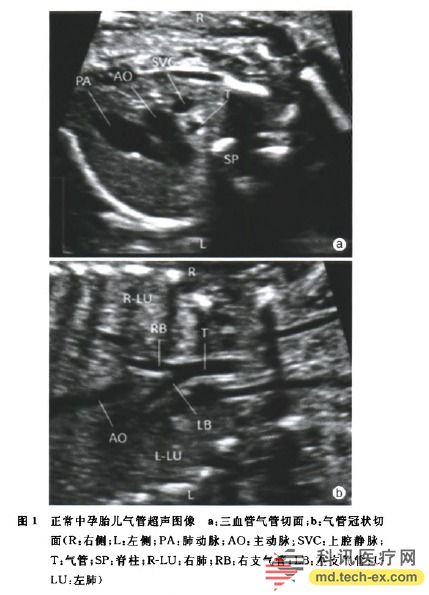
On the trivascular tracheal section, the fetal trachea appears as a round-like strong echo, located posterior between the aortic arch and the superior vena cava (Fig. 1a). On the tracheal coronal section, the trachea and the bronchus on both sides are inverted (Y-shaped) (Fig. 1b), and the left and right bronchus can be traced into the hilum.
Grange et al. used pulsed Doppler ultrasound to observe the flow of liquid in the trachea during normal fetal breathing. It was found that the flow rate of the fluid in the trachea was increased when the normal fetus inhaled, and the flow rate during exhalation was slowed down. Nakai et al. used pulsed Doppler ultrasonography to observe the peripheral bronchial fluid flow in 28 normal fetuses aged 32-38 weeks. It was found that when the fetus was breathing, the fluid flowed into the bronchus of the lung segment, and the flow velocity of the fluid in the bronchus could be measured. .
The results show that Doppler ultrasound can observe fetal respiratory movements in a non-invasive and semi-quantitative manner, which may provide a new perspective for better defining the degree of lung dysplasia in the future.
There are few reports on the ultrasound display rate and measurement of normal fetal trachea, and the views are not consistent. Wolfson et al. performed ultrasound on the trachea of ​​25 fetuses. The tracheal display rate was 80.0%. It was considered that the fetal tracheal diameter did not change significantly with the increase of gestational age. Richards et al reported that the display rate of 120 normal fetal trachea was only 47.0%; the mean tracheal diameter was 2.4 mm at 18 weeks of gestation and 4.6 mm at 38 weeks of gestation.
Kalache et al. performed ultrasound measurements on 198 cases of fetuses aged 15-40 weeks. The measured section was: the head of the fetus was shown to pass through the front of the trachea, and the medial edge of the trachea was measured to the contralateral side of the trachea. As a tracheal diameter, the results show that ultrasound can clearly show the fetal trachea at around 15 weeks of gestation. Fetal tracheal diameter has a good correlation with gestational age and increases with the increase of gestational age.
Tao Yichao and other methods used the same method to observe and measure the trachea of ​​329 pregnant fetuses aged 16-36+6 weeks. The tracheal display rate was 82.0%. The best period for prenatal ultrasound showed fetal trachea was 21-30+6 weeks. It was confirmed that the development of trachea was linearly related to gestational age.
Advances in ultrasound diagnosis of congenital tracheal and bronchial lesions
1. Congenital tracheal dysplasia / atresia: In 1962, Floyd et al. classified congenital tracheal dysplasia based on the growth and development of trachea and bronchus and whether or not combined with esophageal fistula. Type I refers to partial obstruction of the trachea, and the bronchus and a small portion of the distal trachea are normal, with tracheal esophageal fistula. Type II refers to the complete obstruction of the trachea, and the trachea and bronchus are normal, and the tracheoesophageal fistula is not combined.
Type III means that there is no trachea, the bronchi is directly emitted from the esophagus, and the connection between the bronchi and the esophagus is often regarded as a bronchial esophageal fistula. The cause of tracheal dysplasia with esophageal fistula may be related to the same diverticulum that originated in the original pharyngeal cavity. The incidence of tracheal dysplasia is <1/50 000, mainly male. The incidence rate of sibling siblings is 1%.
Serious symptoms such as vocalization and cyanosis appear during childbirth. After receiving airway respiration support, the newborn still has respiratory distress and difficulty breathing. Therefore, the fetus generally cannot survive after birth. Prenatal ultrasound is helpful in diagnosing the disease. The onset may be related to excessive or too little amniotic fluid.
Lupi et al reported a case of a 34-week-old fetus. Ultrasonography showed excessive amniotic fluid, intrauterine growth restriction and ascites. The tracheal trunk was short and had a length of about several centimeters. The bronchus and enlarged unilateral dilatation were seen below. The lungs are connected, the ultrasound is suspected of tracheal malformation; the fetus has no crying and spontaneous breathing after delivery; the autopsy shows that the trachea is 3 cm long, the distal end terminates at a blind end, and the lungs swell and connect through a thin-walled bronchus, which is diagnosed as " Tracheal atresia."
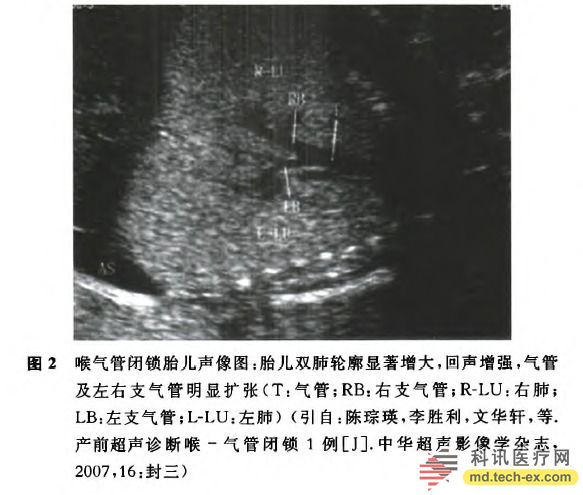
Lacy et al reported two cases of fetal cases. Prenatal ultrasound showed strong echoes of bilateral lung expansion, accompanied by pleural and abdominal effusion and skin edema. Post-mortem autopsy confirmed tracheal atresia. Chen Wei et al reported a case of ultrasound diagnosis of laryngotracheal atresia. Ultrasound showed that the two lungs of the fetus were significantly dilated, and the middle and lower trachea of ​​the trachea were significantly dilated (Fig. 2). The connection between the upper end of the trachea and the throat was unclear, with edema and amniotic fluid. More, after anatomy, it was confirmed by anatomy.
Shi Weiyuan et al reported a case of ultrasound suspected fetal tracheal atresia. The sonogram showed a significant increase in bilateral lung symmetry and a high echo. The upper trachea was not shown, the middle and lower segments were dilated (about 4.6 mm) with edema, and autopsy confirmed tracheal atresia. Summarized the literature to obtain the ultrasound manifestations of fetal tracheal atresia: 1 bilateral lungs are more symmetric expansion, echo enhancement; 2 tracheal echo is interrupted, distal visible expansion; 3 often combined with polyhydramnios, too little and fetal edema; 4 combined esophagus When the sputum is present, the gastric vesicle may be too small or not displayed.
2. Congenital bronchial atresia: This disease is a rare congenital dysplasia. The lesions occur mostly in the segmental or sub-segmental bronchus. The pathology is local occlusion or stenosis of the proximal luminal, and the bronchial mucus-occlusive cyst with normal distal development. It forms a dilated bronchial structure containing gas and liquid at the same time as the residual inflatable void. Ultrasound diagnosis of fetal bronchial atresia is not uncommon, but most cases are reported.
McAlister et al reported a congenital right main bronchial atresia and tracheal stenosis in the fetus. The 24th week of the sonogram showed a right lung dilatation, a mass in the lung (with two small echo-free areas), bronchiectasis and lumen It is filled with anechoic mucus. As the gestational age increases, the size of the mass does not change much. The small anechoic area increases gradually. The child has severe respiratory distress after birth. The autopsy shows tracheal stenosis and right main bronchial atresia.
Kamata et al reported that in a 32-week ultrasound examination, a cyst was found in the left lung of the fetus. At first, it may be congenital lung adenomatoid malformation, isolated lung or bronchial cyst; in subsequent follow-up observation, there was no significant change in cyst size. Newborns did not have respiratory symptoms and related signs after birth. Chest CT showed left atelectal atelectasis and cysts with a diameter of about 15 mm. Fibrobronchoscopy revealed a left upper segment of the bronchus, followed by a diagnosis of left upper segment bronchial atresia.
Bonnefoy et al reported 3 cases of fetal bronchial atresia in the lungs. The common ultrasound findings were: strong echoes in the lungs with enlarged lesions, full airway expansion and no echo in the lungs, mediastinal shift, healthy lungs and lateral diaphragmatics. Pressure.
One of the fetuses was complicated with ascites and polyhydramnios. The fetal lung weight ratio of 3 cases was always lower than 0.015, suggesting severe lung dysplasia. After autopsy after induction of labor, it was confirmed that there were 1-2 lobe bronchial atresia in 3 fetuses, and the lungs of the lesions were enlarged, resulting in the remaining normal lung lobe, contralateral lung and heart were compressed.
Abitayeh et al reported two cases of premature three-dimensional ultrasound diagnosis of bronchial atresia. Two cases of fetal two-dimensional ultrasound showed: the expanded right lung showed strong echo, the mediastinum was biased to the left, edema and polyhydramnios. One of the patients had a suspected type III cystic adenomatoid malformation before the fetus, but three-dimensional ultrasound showed the expanded right bronchus and was confirmed by autopsy.
Another case of fetal three-dimensional volume contrast imaging examination also found the expansion of the right main bronchus, thus determining the diagnosis of the main bronchial atresia. At the same time, it is considered that the main bronchial atresia is more serious than the bronchial atresia and bronchial atresia in the lung segment. Three-dimensional ultrasound imaging is helpful for prenatal diagnosis of fetal bronchial atresia.
Through the above case analysis, the ultrasound image of fetal bronchial atresia can be roughly summarized: 1 the affected lung enlarges or shows strong echogenic mass; 2 the affected bronchial segmental dilatation shows no echo; 3 mediastinum, healthy lung and transverse膈 under pressure displacement; 4 as above ultrasound signs and lung cystic adenomatoid malformation and isolation of the lungs are very similar, need to be identified; 5 often with lung dysplasia, polyhydramnios or ascites.
3. Congenital tracheal stenosis: Deletion of the tracheal membrane can result in local or most stenosis of the trachea. Backer et al believe that the anatomical diameter of the trachea is less than one-half of the normal trachea, which is tracheal stenosis, and more than half of the congenital tracheal stenosis will be combined with other malformations. Distal airway stenosis may be associated with left pulmonary artery abnormalities, such as pulmonary sling deformities or complex annular slings, which can cause compressional stenosis of the trachea.
Therefore, when the pulmonary artery sling deformity is found by ultrasound, the possibility of distal tracheal stenosis should be guarded. At present, there are few reports in related literatures. McAlister et al reported in the study of cases of tracheal stenosis by ultrasound, but did not directly observe the signs of tracheal stenosis, but found abnormal echoes in the lungs, and confirmed postpartum autopsy.
4. Tracheobronchial disease: Most of the disease is congenital, but generally until the middle age period, there are obvious symptoms, the pathological changes are mainly the loss of tracheal muscle. Enriquez et al reported that after intrauterine endoscopic treatment of congenital diaphragmatic and pulmonary dysplasia, the inner diameter of the tracheobronchial is larger than the normal fetus of the same age group, which may be due to mechanical damage to the tracheal wall. With the development of intrauterine treatment of fetal diseases, prenatal ultrasound has found that the disease may gradually increase.
5. Congenital high airway obstruction syndrome: This disease is a rare fetal malformation with low survival rate, which can be caused by tracheal dysplasia or atresia, laryngeal atresia, huge laryngotracheal cyst and subglottic stenosis.
Prenatal ultrasound if the bilateral symmetry of the enlarged lung echo, mediastinal compression or displacement, airway dilatation and mediastinal compression, ascites or amniotic fluid, is a sign of complete or near complete fetal airway obstruction . Congenital high airway obstruction syndrome can be diagnosed when the above-mentioned prenatal ultrasound signs are combined with fetal edema.
Fifth, the role of bronchial morphology in judging fetal visceral azimuth
The fetal visceral orientation is divided into three types: visceral orthodontic position, visceral inversion and visceral non-position. At present, the ultrasound determines the fetal visceral orientation and uses the method of adult ultrasound, that is, according to the position of the abdominal visceral and large blood vessels, and the ultrasonic diagnosis method of the chest organ orientation other than the heart has not been reported yet.
Anatomical studies confirmed that when the visceral position was normal, the left lung was two leaves, the right lung was three-leaf; the left bronchus was slender, the right bronchus was thick and short, and the ratio of the length of the two was >1.5-2; the right bronchus was in the right pulmonary artery. Upper left bronchus runs under the left pulmonary artery. When the plexus of the thoracic organ is ectopic, the ratio of the length of the bilateral bronchus is about ≤1.5 in about 90% of the cases, and the relationship between the bronchus and the branch of the pulmonary artery changes in 95% of cases.
Among them, on the right side, the bilateral side is often a three-leaf lung, the bilateral side is mostly the shape of the right bronchus, both sides of the bronchus are walking on the ipsilateral pulmonary artery; while the left side is often bilaterally two-leaf lung. Both sides are mostly left bronchial, and both bronchial tubes are under the ipsilateral pulmonary artery.
It can be seen that the morphology of the bronchi and its relationship with the peripheral blood vessels are important anatomical landmarks for determining the orientation of the thoracic organs. If the ultrasound morphological features of the fetal bronchus can be studied, and the relationship between the bronchus and the surrounding structure can be determined, it may provide a new perspective for determining the fetal visceral orientation.
In summary, ultrasound can show the trachea and main bronchus of normal fetuses. Related lesions also have obvious ultrasound changes, such as enlarged lung or mass echo, distal bronchiectasis, accompanied by edema and amniotic fluid changes, but need to be differentiated from cystic adenomatoid malformation and isolated lung . More attention during prenatal ultrasound examination can improve the detection rate of tracheal and bronchial lesions.
Article from "Chinese Journal of Ultrasound Imaging", June 2014, Vol. 23, No. 6, P535 - 537
Author: Wu Ying Yin Shao Li
Source: Chinese Journal of Ultrasound Imaging
Wireless Camera Kits With 4 Camera
We are manufacturer of Wireless Camera Kits With 4 Camera in China, if you want to buy Wireless 1080P Security Camera System please contact us.
The IOT card of the video surveillance camera needs to be stable enough to keep the flow normal during use without being stopped. After using the IOT network card with defective quality for a period of time, traffic theft or other abnormal conditions suddenly occur, resulting in card suspension, which makes the camera terminal unable to use normally, and may have a significant impact on the business. Generally speaking, video monitoring is event driven or abnormal images (some intelligent algorithms need to be supported) to generate high traffic usage. For example, monitor video playback or live broadcast via 4G/5G remote viewing. Generally, the daily standby traffic consumption is M, and the common definition of video viewing is about hundreds of M an hour.
Currently, for this application scenario, there are also several industry pain points for equipment manufacturers and solution providers:
SIM card adaptation, speed and security issues;
SIM card supply and price stability;
Be unfamiliar with the communication industry and solve the problem of failure;
One point access of multiple vendors.
Honeycomb IoT provides high-speed and stable IoT network cards for security monitoring equipment. Direct connection of operators, including full system, full type and full category IoT SIM cards; Flexible pricing and high cost performance; In addition, it also has a customer oriented efficient management platform, including full lifecycle management and connection management functions.
Wireless Camera Kits With 4 Camera,Wireless 1080P Security Camera System,Wifi Surveillance Camera System,Wireless Security Camera System
Shenzhen Fuvision Electronics Co., Ltd. , https://www.outdoorsolarcameras.com